1 Folly of surrogates
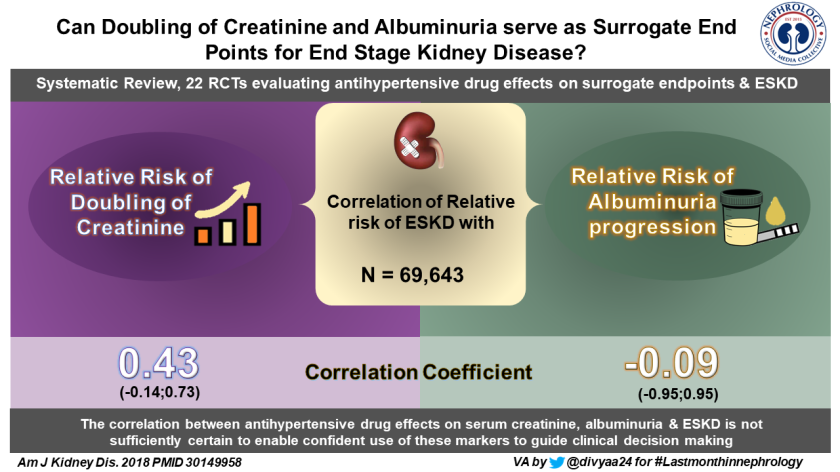
Visual abstract by Dr. Divya Bajpai (@divyaa24)
Whether its phosphorus, blood pressure, PTH, or albuminuria- the numbers guide us all in our practice. Being easily modifiable with treatments, surrogates are attractive outcomes not only in nephrology but also in other areas of medicines. However, more often than not, that’s not what patients want from us. They want us to improve the way they ‘feel, function and survive’. Here is something that highlights this once again for us: in a meta-analysis of BP lowering treatment trials (22 trials involving 69,642 participants), there was limited correlation between drug effects on surrogates (albuminuria, eGFR/creatinine) and risk of ESRD.
These findings contrast the NKF and USFDA’s view that proteinuria is a reliable surrogate of kidney disease progression. For decades, we have been deluded by surrogates, not surprisingly, we see dissociation between soft endpoints and patient-centered outcomes. Are CANVAS, EMPAREG, and LEADER listening?
2 Biocompatible Solutions and Long-Term Changes in Peritoneal Solute Transport
Speaking of surrogate endpoints, if faster peritoneal solute transport rate is associated with poor outcomes(read technique failure and mortality and encapsulating peritoneal sclerosis), a fluid that preserves the transport characteristics of the peritoneal membrane would be an ideal PD solution.
Elphick et al analyzed the data from the multinational prospective Global Fluid Study to test the hypothesis that biocompatible solutions use would be associated with stable membrane function. This hypothesis proved false, because “solute transport rate, although starting slower in patients using biocompatible solutions, rose to similar levels seen in standard solutions after 2 years of treatment. After 2 years, there was a potentially beneficial effect of biocompatible solutions on solute transport rate, with abrogation of the increases in solute transport rate observed in patients using standard solutions. In addition, the increases in solute transport rate associated with peritonitis episodes were absent in patients using biocompatible solutions. The magnitude of these effects was less than the effect of using higher dialysate dextrose concentrations.” There may be a long-term benefit; only a large study with long-term follow up would tell us that.
3 Uric acid lowering and CKD progression

Visual abstract by Dr. Aakash Shingada (@aakashshingada)
Monsoon is the lifeblood for Indian farmers and it regularly defies meteorological department’s predictions, so much so that some farmers recently filed a police complaint against the department and a farmers’ organization had threatened to close down their office. We desperately need a better tool to predict rains. In absence of such a tool, some farmers look at the height at which a weaver bird builds its nest on a tree to predict the rains. I find myself in no better position when a patient with CKD (especially those with no significant HTN and proteinuria) asks me about the future course of his disease and if I would be able to change the trajectory in a better way. Uric acid, for some of us, is that weaver bird’s nest.
In the multicenter, placebo-controlled, double-blind, FEATHER (Febuxostat Versus Placebo Randomized Controlled Trial Regarding Reduced Renal Function in Patients With Hyperuricemia Complicated by Chronic Kidney Disease Stage 3). Compared to placebo, febuxostat did not mitigate the decline in kidney function among patients with stage 3 CKD and asymptomatic hyperuricemia. Not convinced by the futility of this therapy, the authors try and speculate on various reasons for the negative results of the trial like higher eGFR (65-year-old, eGFR, and stage 3 CKD—you know what I mean), a generally slower decline of eGFR in their patients, no significant proteinuria etc. Diastolic BP was lower in the febuxostat group (not surprising as they were more likely to be on ACEi/ARBs)
Only thing I am sure about febuxostat today is that it’s an effective urate-lowering agent and FEATHER just confirms this observation.
4 TRANSFORMing long-term outcome after kidney transplantation, really?
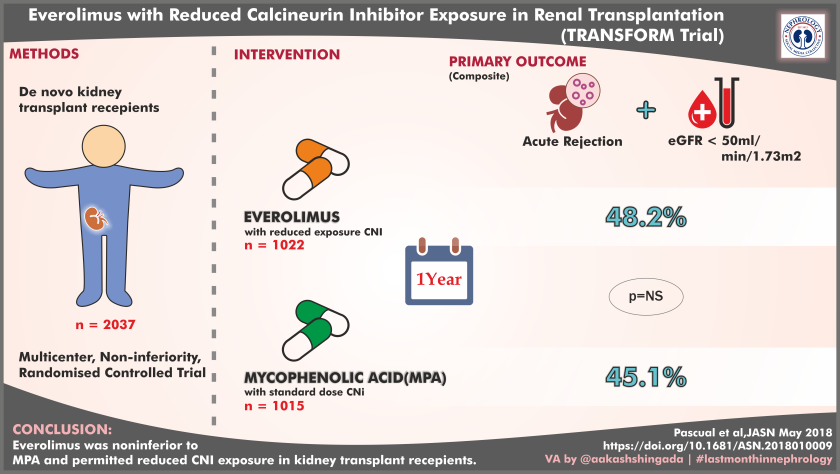
Visual abstract by Dr. Aakash Shingada (@aakashshingada)
Set out to address the burning issue of chronic allograft injury, here is a report (yet another), an RCT comparing everolimus with reduced CNI exposure with conventional immunosuppression i.e. MMF with standard CNI dosing (arguably TAC trough levels of 8-12 vs 3-8 in everolimus arm will qualify for ‘high dose CNI’ strategy). Everolimus arm was non-inferior to conventional arm for the primary endpoint which was (novel according to Novartis): binary composite of tBPAR(treated biopsy-proven acute rejection) or eGFR<50 ml/min at 12 months post-transplant [48.2% (493) with everolimus and 45.1% (457) with MPA (difference 3.2%; 95% confidence interval, 21.3% to 7.6%)]. Infections (especially CMV and BKV) were less common in everolimus arm.
Are you ready to get transformed? You may if you are willing to forgo the following flaws: the fallacy of eGFR as efficacy endpoint, generous 10% noninferiority margin, two components of the binary endpoints not necessarily changing linearly, and exclusion of high-risk patients. Also please let go of the tolerability-mTOR arm was more than two times likely to discontinue medication due to side effects (23% vs 11.9%). So we are no further than this Cochrane review as of now.
When will we move to patient-centered research in transplantation? Neither I nor my patients will be ready to get transformed just by good-looking numbers at 12 months. They deserve much more than that.
5 Patient-Reported Experiences of Dialysis Care
Moving away from surrogates, here is an interesting report of patient-reported experiences of dialysis care patients from a national ESRD registry receiving in-center hemodialysis in the United States. In-Center Hemodialysis Consumer Assessment of Healthcare Providers and Systems (ICH-CAHPS) survey, (this contains questions like-how often did you feel your kidney doctors really cared about you as a person? never/sometimes/usually/ always).
2939 (59.1%) reported mean ICH-CAHPS scores. Patient experience of the dialysis centers was poor (lower ICH-CAHPS score) if the center has the following characteristics: for-profit units, stand-alone centers, fewer nurses and technicians per patient, centers belonging to LDO (Large Dialysis Organisation), had more patients with minority race/ethnicity.
Although limited by various factors (39% centers didn’t report, the interplay of medical and nonmedical factors etc), this exercise should be done more and more often to better understand the gaps in the delivery of complex treatment like dialysis. Inputs derived can potentially help improve the quality of dialysis care.
6 What happens when hemodialysis is free of cost?
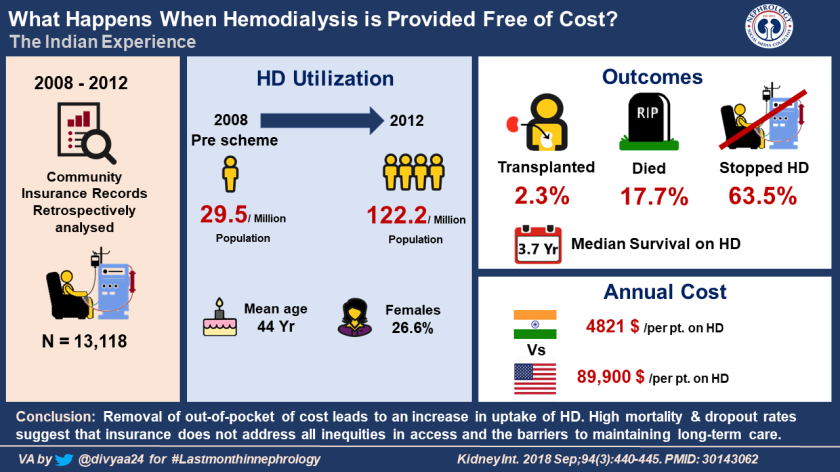
Visual abstract by Dr. Divya Bajpai (@divyaa24)
While patient-reported experiences of care may be less favorable in for-profit hemodialysis units, a paper published from India enlightens us about a government-sponsored program where patients are provided maintenance hemodialysis free of cost. Andhra Pradesh, a southern state in India, implements the Rajiv Aarogyasri Community Health Insurance Scheme (RACHIS) where a private insurer provides a health insurance and is paid in full by the state government. Beneficiaries are able to utilize hospital services through a network of public and private hospitals and are covered up to INR 150,000 ($ 8876) per year.
A total of 13,118 patients received HD for ESRD during the study period (mid-2008-mid-2012). The program had a good reach and the number of patients who received HD for ESRD increased from 29.5 per million of the population in 2008–2009 to 122.2 per million of the population in 2011–2012.
Of all the subjects who started HD, 2.3% received a kidney transplantation, 17.1% were reported as dead, and 63.5% had ceased treatment of their ESRD (i.e., stopped reporting to dialysis centers).
The total cost of HD-related care was $ 63.2 million. The mean annual expenditure per patient on HD-related care was $ 4821. (This contrasts with $ 89,900 in the United States!)
Costs other than dialysis costs (commuting, loss of wages, drugs, caregiver burden) could be the reason for the high dropout rate; but what is most striking here is the high mortality rate.
Maintaining low-cost services alone is not enough; the model must have in-built checks to improve the outcomes.
In authors’ word, “In conclusion, removal of out-of-pocket of cost leads to an increase in uptake of HD, confirming a previously high unmet need. The high mortality and dropout rates suggest that insurance coverage does not address all inequities in access and the barriers to maintaining long-term care.”
[Let me thank Dr. Krishna Penmatsa (@krishnadoctor1) who gave me insights into the Rajiv Aarogyasri Community Health Insurance Scheme (RACHIS)]
Monitoring the urine flow to prevent overcorrection of hyponatremia
Urine output is probably the most important parameter to monitor when one treats hyponatremia; arguably more useful at the bedside than urine lytes and osmolality (given the typical turnaround time). Once the component of volume contraction (or whatever is the cause of high ADH level) is taken care of, the stimulus for ADH secretion is taken away and this leads to water diuresis leading to a rapid rise in serum sodium. The best strategy at our disposal is frequently checking the sodium level (and using DDAVP of course).
If you are a nephrologist, you must read (and pretend that you understood every single word of it) this article published in AJKD last month. Florian Buchkremer et al have derived on theoretical grounds a safe upper limit of urine flow, dependent only on body weight, that can be easily used at the bedside.
Edelman is the root of almost all good in nephrology. Based on the Edelman equation, authors suggest using a urine flow rate of 24 mL/kg/24 h or 1 mL/kg/h (up to a maximum of 2,400 mL/24 h or 100 mL/h) as a safe upper limit during correction of hyponatremia.
If you have been called for a hyponatremia consult and are seen doing narcissistic calculations trying to predict the next morning’s sodium and find that you are terribly wrong, you are welcome to the club! Discrepancies between actual plasma sodium changes and those predicted by the Edelman equation have been reported, but most of that is related to the things we assume. The equation stands tall! But one thing we can take from this paper is the order we are going to write- “Document total urine volume [as voided or every 2 hours in patients with catheters]. Notify the treating physician as soon as the cumulatively voided volume exceeds 6mL/kg in 6 hours.”
